Your basket is currently empty!
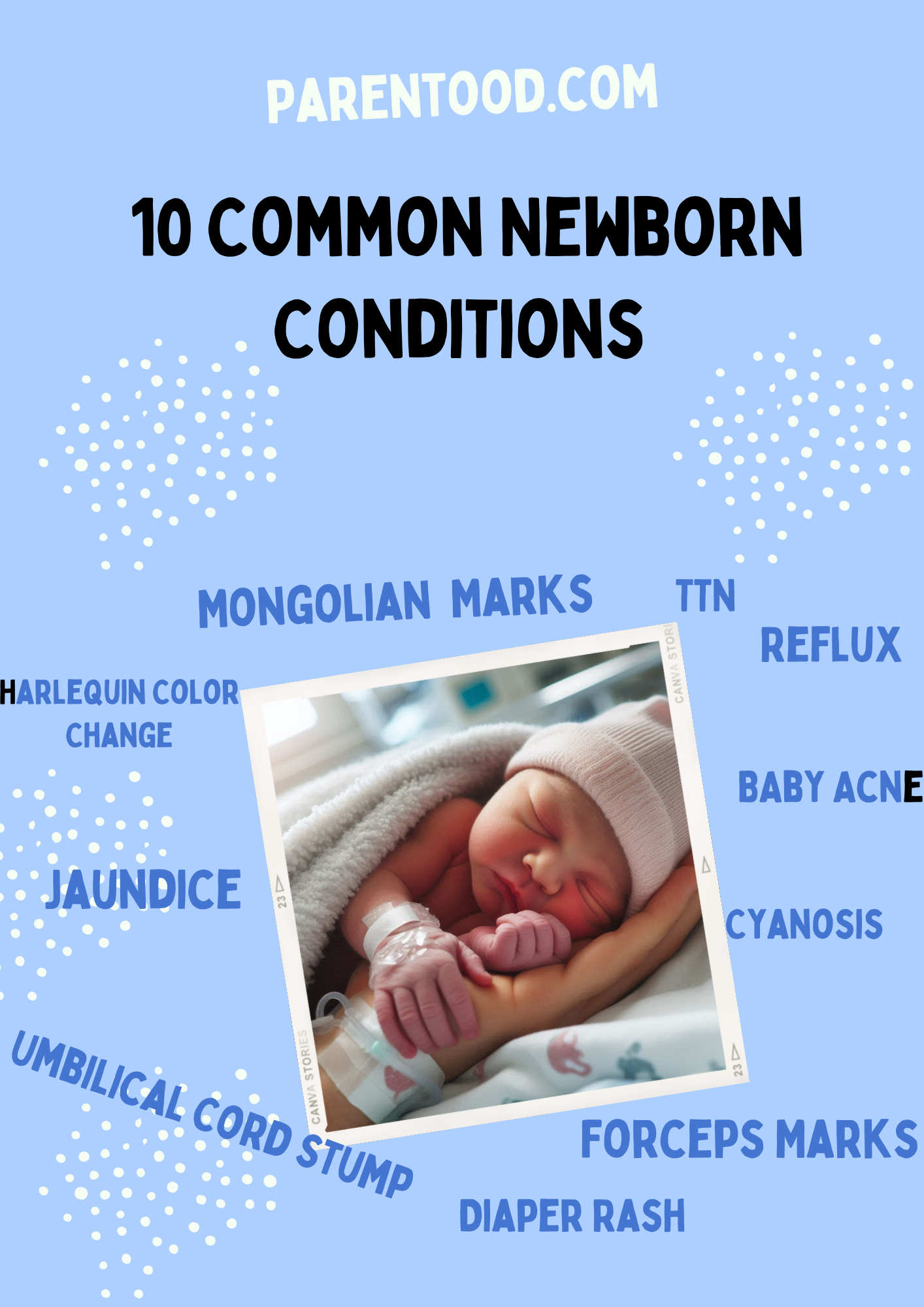
10 Common Newborn Physical Conditions
Newborns often experience several physical conditions during the first few weeks after birth, most of which are normal and resolve on their own. Common issues include jaundice, forceps marks, Mongolian spots, mild cyanosis (“blue baby”), and conditions like spitting up or transient breathing issues. Skin concerns like baby acne, diaper rash, and temporary color changes are also frequent. While most conditions require minimal treatment, some signs—like persistent jaundice, severe rashes, or central cyanosis—warrant medical attention. Understanding these common newborn conditions can help parents distinguish between normal developmental changes and signs that need further evaluation by a healthcare professional.
The first couple of weeks after birth is a period of significant adjustment for a newborn. During this time, it’s normal for babies to go through several physical changes and exhibit certain conditions. Most of these are typical and resolve on their own, but some might require closer attention. Below are some common physical conditions that newborns might experience, explanations for each, and indicators of when to seek medical help:
1. Jaundice
- What it is: Jaundice is the yellowing of a newborn’s skin and eyes due to high levels of bilirubin. Newborns have a higher turnover of red blood cells, and their immature liver may not process bilirubin efficiently.
- Common Symptoms: Yellowish tint to the skin and whites of the eyes, starting on the face and moving down to the chest.
- When to get worried: If jaundice appears within the first 24 hours, spreads to the arms and legs, or lasts longer than two weeks. Additional warning signs include poor feeding, excessive sleepiness, or dark urine.
- Treatment: Mild jaundice often resolves on its own. More severe cases may require phototherapy (light therapy). In rare situations, an exchange transfusion is needed.
2. Forceps Marks
- What it is: These are temporary marks or bruises left on the baby’s face or head after a forceps-assisted delivery. Forceps are sometimes used if labor is complicated or prolonged.
- Common Symptoms: Red marks, slight bruising, or indentations on the cheeks or scalp. Swelling in the affected area is also common.
- When to get worried: If the marks don’t improve over a week or seem to worsen, or if the baby appears to be in pain or has difficulty moving the facial muscles. Seek medical attention if the bruising is accompanied by swelling or if you notice any open wounds.
- Treatment: Usually no specific treatment is required, and marks fade on their own within a week or two. Cold compresses can help with swelling, and medical follow-up may be necessary if there are deeper injuries.
3. Mongolian Spots
- What it is: These are bluish-gray birthmarks that look like bruises and are caused by pigment cells trapped in deeper layers of the skin. They are more common in babies with darker skin tones.
- Common Symptoms: Bluish or gray patches, usually on the lower back, buttocks, or sometimes on the arms and legs. They are flat and do not cause pain or discomfort.
- When to get worried: Mongolian spots are harmless and not linked to any medical issues. If they do not fade by early childhood, mention it to your pediatrician, but they are not dangerous.
- Treatment: No treatment is needed; they generally fade on their own by the age of 4 to 5 years.
4. Blue Baby Syndrome (Cyanosis)
- What it is: Cyanosis refers to a bluish tint to the skin, especially around the lips, hands, and feet. It is often due to poor oxygenation in the blood. In newborns, mild cyanosis in the hands and feet (called acrocyanosis) is normal in the first few days after birth. However, cyanosis involving the lips, tongue, or central body can indicate a serious underlying issue.
- Common Symptoms: Blue or gray discoloration, particularly in the face, lips, and fingernails. Breathing might be rapid or labored, and the baby may seem lethargic.
- When to get worried: If the bluish tint persists, spreads, or affects the central areas (like the chest or face), it could signal a heart or lung problem. Seek immediate medical attention if cyanosis occurs with difficulty breathing, feeding problems, or lethargy.
- Treatment: Depends on the cause. Mild acrocyanosis usually resolves as the baby’s circulation improves. Central cyanosis requires urgent evaluation and possibly hospitalization to assess the heart and lungs. Treatment can involve oxygen therapy, medications, or in severe cases, surgery.
5. Spitting Up / Reflux
- What it is: Spitting up is common due to an immature digestive system and the baby’s short esophagus. Most babies spit up occasionally, which is generally harmless.
- Common Symptoms: Small amounts of milk regurgitated after feeding, particularly when burping.
- When to get worried: Seek medical help if the baby isn’t gaining weight, has projectile vomiting, appears to be in pain, or spits up green/bloody fluid.
- Treatment: Holding the baby upright after feeding, burping frequently, and feeding smaller amounts more often can help. Severe reflux might require medication.

6. Transient Tachypnea of the Newborn (TTN)
- What it is: A condition where newborns breathe faster than normal due to fluid remaining in the lungs after birth. It’s more common in babies born via cesarean delivery or rapid vaginal deliveries.
- Common Symptoms: Rapid breathing (more than 60 breaths per minute), grunting, and slight chest retractions.
- When to get worried: If fast breathing doesn’t improve within a day or two or if it’s accompanied by severe respiratory distress, such as nostril flaring or turning blue.
- Treatment: TTN typically resolves on its own within 48-72 hours. Monitoring oxygen levels and supportive care (like supplemental oxygen) may be needed in the hospital.
7. Umbilical Cord Stump Care
- What it is: After birth, the umbilical cord is clamped and cut, leaving a small stump. This stump dries up and falls off within 1-2 weeks.
- Common Symptoms: The stump will darken, shrink, and eventually fall off. A small amount of dried blood is normal.
- When to get worried: If the area around the stump is red, swollen, or has a foul odor, or if there’s pus-like discharge, it could indicate an infection. Seek medical care if the baby develops a fever.
- Treatment: Keep the stump clean and dry, avoid submerging it in water, and fold diapers below the stump to allow air to circulate. Mild antiseptic may be used if advised by a doctor.
8. Baby Acne and Milia
- What it is: Tiny pimples or white bumps that appear on the baby’s face due to hormones or blocked pores.
- Common Symptoms: Red or white bumps on the cheeks, forehead, or chin. Milia are tiny white bumps caused by blocked oil glands.
- When to get worried: Baby acne is harmless and does not require treatment. If the rash spreads significantly, becomes very inflamed, or if there are other signs of illness like fever, consult a doctor.
- Treatment: No treatment is needed, as both baby acne and milia clear up on their own within weeks.
9. Diaper Rash
- What it is: Diaper rash is an irritation of the skin caused by prolonged exposure to moisture, friction, or irritants in diapers.
- Common Symptoms: Red, irritated skin in the diaper area, possibly with small bumps or scaly patches.
- When to get worried: If the rash is severe, spreads, or has blisters, or if it doesn’t improve with regular care. A fungal or bacterial infection may be present if it persists.
- Treatment: Keep the diaper area dry, change diapers frequently, and use a barrier cream like zinc oxide. Air time without diapers can help. For severe cases, antifungal or antibiotic creams may be needed.
10. Transient Skin Color Changes (Harlequin Color Change)
- What it is: A harmless, temporary change in skin color where one half of the baby’s body appears redder than the other, often when lying on one side.
- Common Symptoms: A noticeable difference in skin color on one side of the body, with a clear line down the middle. This change can last from a few seconds to a few minutes.
- When to get worried: It’s generally harmless. However, if it persists or you notice other unusual symptoms like difficulty breathing or feeding, consult a doctor.
- Treatment: No treatment is necessary. This resolves as the baby’s circulation matures.
Conclusion
Most of these conditions are common and normal adaptations to life outside the womb. Monitoring for signs of discomfort or distress is key. In any case where the baby’s symptoms seem severe, persistent, or concerning, always consult a pediatrician for further evaluation and guidance.

Leave a Reply